Introduction:
Bleeding disorders in women, particularly in developing countries, have been largely neglected due to various factors such as social stigma, limited access to comprehensive laboratory facilities, and the misconception of physiological bleeding during menstruation. Heavy menstrual bleeding (HMB) is a common symptom in women, and a significant percentage of cases may be associated with inherited bleeding disorders. However, the underreporting and underdiagnosis of these conditions remain prevalent, partly due to the stigma surrounding menorrhagia, leading to delayed medical care seeking. This study aims to explore the clinical and laboratory profiles of females with bleeding disorders who presented to our institute.
Methods:
A consecutive series of female patients referred to our advanced coagulation laboratory for complete workup with bleeding manifestations or abnormal screening coagulogram over a 59-month period (September 2018 to July 2023) were assessed. Patients with liver disease, chronic inflammation, or on anticoagulation therapy were excluded. Data on age at presentation and diagnosis, ISTH BAT score, annual bleeding rate, family history, hospitalizations, surgical interventions, and follow-up were retrospectively retrieved from our database. Heavy menstrual bleeding was subjectively defined based on specific criteria. Various laboratory parameters were analyzed for all patients. Data were presented using median/range and percentage. Missing data were not imputed, and MS Excel 2016 was used for analysis.
Results:
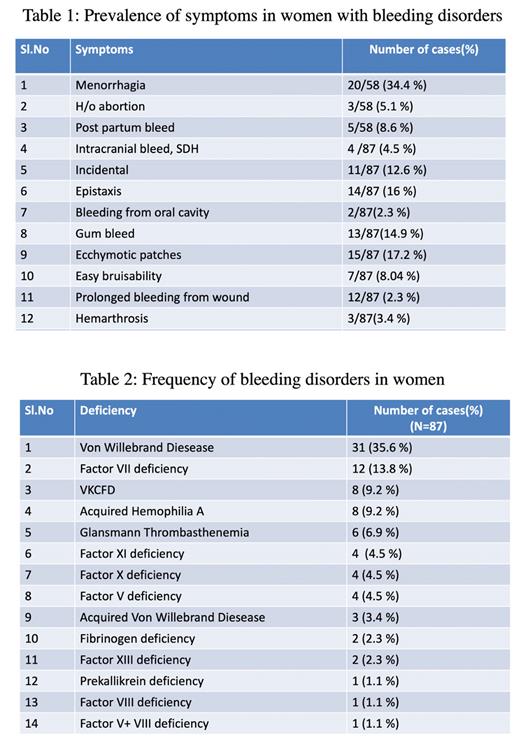
Over the study duration, 1019 patients were evaluated at our institute, with 488 females (47.9%) and 531 males (52.1%). Among the 235 patients (23%) diagnosed with bleeding disorders, 87 (37%) were women. The median age at diagnosis was 29 years (range: 9 months-84 years), while the median age of first symptom was 15 years (range: 7 days-81 years). The median time interval between presentation and diagnosis was 8 years (range: 6 months-30 years). The most common presenting symptom was HMB (34.4%), followed by ecchymotic patches (17.2%) and epistaxis (16%). Significant ISTH BAT scores (>6) were found in 17 patients (19.5%). A family history of bleeding was observed in 4.5% of patients, with 3 of them born to consanguineous parents. Incidentally detected abnormal screening coagulogram was present in 12.6% of patients. The most common bleeding disorder diagnosed was VWD (35.6%), followed by Factor VII deficiency (13.8%), Vitamin K dependent coagulation factor deficiency (9.2%), and Acquired Haemophilia A (9.2%). Intracranial bleeding (4.5%) was primarily associated with specific deficiencies. No carriers were detected in the study.
Conclusion:
Addressing bleeding disorders in women requires specific attention. The ISTH BAT score proved to be a user-friendly yet powerful tool, with 19.5% of patients showing significant scores that prompted comprehensive diagnostic workup. This study highlights the long latent period between the age of first symptom and the age of diagnosis, emphasizing the need to raise awareness among patients and primary physicians, especially gynaecologists. Menorrhagia starting from menarche was the most common bleeding symptom, emphasizing the importance of prompt and accurate diagnosis to prevent life-threatening bleeds. The consideration of acquired hemophilia A is crucial in cases of unexplained postpartum hemorrhage. Developing countries face additional challenges due to limited specialized laboratories, leading to outsourcing and increased testing costs. To improve diagnosis and care, early identification of female bleeders is essential, facilitated by outreach programs and advanced coagulation testing centers.
Disclosures
No relevant conflicts of interest to declare.